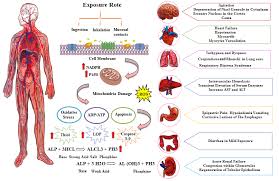
Clinical presentation of aluminum phosphide poisoning
The clinical features of AlPhos poisoning depend on the route, the dose, and the interval between ingestion and presentation. Inhalation of phosphine is a difficult clinical diagnosis, although the smell of rotten eggs or a garlic-like odor may be an important clue.
The most common clinical features include the following: Restlessness, foul garlicky-rotten fish odor, nausea, vomiting, pain abdomen, deep acidotic breathing, tachyarrhythmias and hypotension with maintained consciousness level. The first signs after severe toxicity include refractory hypotension and metabolic acidosis, within the first few hours of admission. The major clinical and laboratory features as per various studies, case reports and unpublished case series include the following:
- Hypotension (SBP <90 mm Hg)
- Tachycardia (HR >120/min)
- Consciousness is not affected.
- Metabolic acidosis (pH 6.8–7.1)
- High lactate levels (>10 mmol/L)
- Hypoglycemia (blood sugar level <80 mg/dL)
- Low ejection fraction (LVEF = 20–35%)
- Arrhythmias (other than sinus tachycardia)
- Hypokalemia (K+ <3 mmol/L)
- Hypomagnesemia (Mg2+ <1.4 mg/dL)
- Significantly raised transaminases (>200 U/L)
Mostafazadeh et al. reported that some degree of methemoglobin production is a usual finding in ALP toxicity. They also reported a significant link between methemoglobin blood levels and mortality. It seems that the reaction of PH3 and oxyhemoglobin is responsible for denaturing its molecule and produce methemoglobinemia. Table 1: Organ specific clinical features of AlPhos
|
System Affected
|
Clinical Features
|
|---|---|
|
Cardiovascular system
|
• Reduced left ventricular ejection fraction to as low as <20%, suggestive of cardiogenic shock. • Arrhythmias: Supraventricular and ventricular tachycardia, atrial fibrillation/flutter, ventricular tachycardia/fibrillation (VT/VF), sometimes bradyarrthmias requiring pacing, QT dispersion.
|
|
Respiratory system
|
Airway irritation, deep rapid acidotic breathing, cough, chest tightness, SPO2 is maintained, unless there are secondary complications like aspiration, ARDS
|
|
Renal System
|
Oliguria and AKI (acute kidney injury)
|
|
Central nervous system
|
• All patients are conscious and are able to tell the complete history. The sensorium is initially normal in most patients, until hypoxia supervenes resulting in altered mentation and delirium • They may have ataxia, numbness, paresthesia, tremors, muscle weakness and diplopia
|
|
Acid base, electrolyte and metabolic disturbance
|
High-anion gap metabolic acidosis: Degree of acidosis depends on severity of toxiceffects. Most admitted cases show a pH of 6.8– 7.15. • Hyperlactemia • Dyselectrolytemia—all types of electrolyte disturbances are reported and nonspecific • Hypoglycemia has been reported and attributed to sustained vomiting and other unknown metabolic disturbances
|
|
Gastrointestinal system
|
Nausea, vomiting, diarrhea, pain in abdomen, mild derangement of transaminases.
|